Cervical cancer is one of the most preventable cancers affecting women today, thanks to the availability of the anti-cervical cancer vaccination. This vaccine plays a vital role in reducing the risk of cervical cancer by protecting against the human papillomavirus (HPV), a common infection linked to nearly all cervical cancer cases.
Understanding the purpose of this vaccine, who should receive it, its benefits, and when to consult a doctor can help women and families take proactive steps toward better health.

Anti-Cervical Cancer Vaccination
Cervical cancer is one of the most preventable cancers affecting women today, thanks to the availability of the anti-cervical cancer vaccination. This vaccine plays a vital role in reducing the risk of cervical cancer by protecting against the human papillomavirus (HPV), a common infection linked to nearly all cervical cancer cases.
Understanding the purpose of this vaccine, who should receive it, its benefits, and when to consult a doctor can help women and families take proactive steps toward better health.
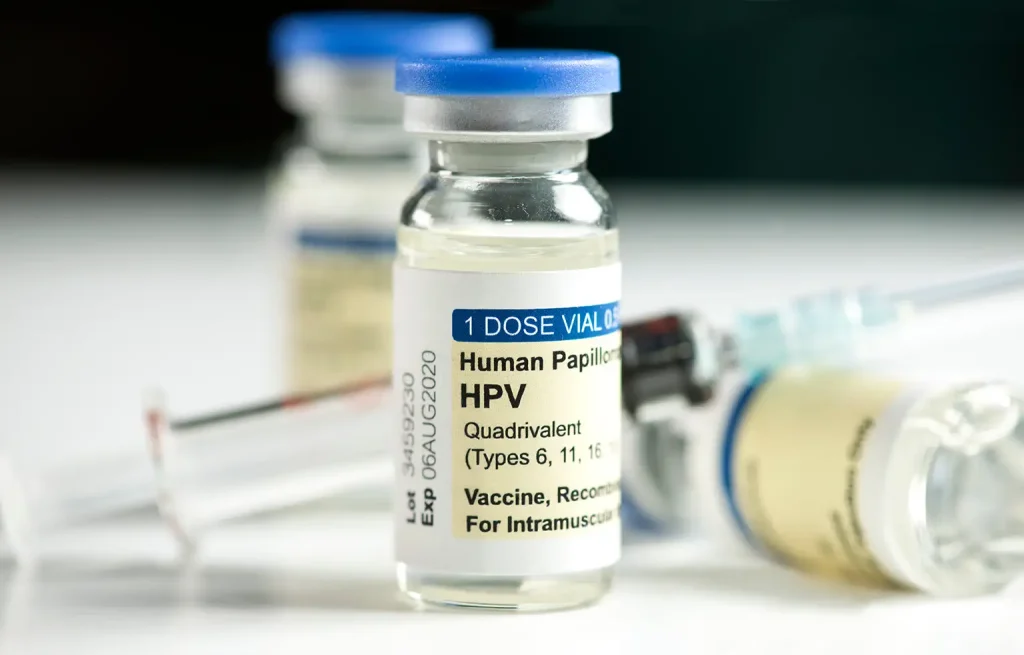
The anti-cervical cancer vaccination is a preventive vaccine that protects against the most common cancer-causing strains of HPV. It targets high-risk HPV strains, particularly types 16 and 18, which cause the majority of cervical cancer cases. These include HPV types 16 and 18, responsible for around 70% of cervical cancer worldwide. HPV is a group of more than 100 related viruses, with certain high-risk types known to cause cervical, anal, vulvar, vaginal, penile, and throat cancers.
There are several approved HPV vaccines on the market. The most widely used is the 9-valent HPV vaccine (Gardasil 9), which protects against nine HPV types, including the high-risk strains responsible for the majority of cervical cancer cases.
There are three main types of HPV vaccines:
The vaccine works by stimulating the body’s immune system to produce antibodies against HPV, preventing future infection.
While the anti-cervical cancer vaccine is preventive, it’s important to be aware of cervical cancer symptoms, especially for those who are unvaccinated or overdue for screening. Symptoms may not appear in the early stages.
Common symptoms include:
Any of these signs should prompt a consultation with a healthcare provider.

Cervical cancer develops over time from long-term infection with high-risk HPV strains. The vaccine is designed to protect against these strains, significantly reducing the risk of cervical and other HPV-related cancers.
Key risk factors include:
Women experiencing any of these symptoms should seek medical care promptly.
Even with vaccination, regular screening is essential for early detection. If HPV is suspected or symptoms appear, a doctor may recommend several tests:
Detects abnormal cervical cells before they become cancerous.
Identifies high-risk HPV types.
A close examination of the cervix if Pap results are abnormal.
Confirms diagnosis by analysing a tissue sample.
Vaccinated individuals may still require screening depending on age and medical history.
The vaccination is a preventive treatment, not a cure. It's most beneficial when administered before sexual debut, but older individuals can still benefit from it.
Yes, the vaccine has been extensively studied and approved by major health organisations worldwide. Minor side effects may include:
Severe reactions are very rare.
You should consult a healthcare provider if:
Early prevention and regular check-ups are key to long-term health.

In Singapore, the HPV vaccine is available under the National Childhood Immunisation Schedule (NCIS) and the National Adult Immunisation Schedule (NAIS). It is also Medisave-claimable at approved clinics and healthcare centres.
At Pacific Healthcare Specialist Centre, we offer:
Speak to our healthcare team about protecting yourself or your child with HPV vaccination as part of cervical cancer prevention.
Contact us to check for a same-day appointment for HPV vaccination.

No, it is also recommended for males to prevent the spread of HPV and related diseases such as genital warts and certain cancers.
Yes. While earlier is better, you can still benefit from the vaccine even after exposure to some HPV types.
Yes. The vaccine does not cover all cancer-causing HPV types, so regular cervical screening remains important.
Serious side effects are very rare. Most people experience only mild symptoms like a sore arm or fatigue.
No. The vaccine is preventive and does not treat existing infections or abnormal cervical cells.
Current research shows long-lasting protection likely over 10 years, with no need for a booster in most cases.
Copyright © 2026 Pacific Healthcare Specialist Centre (Women's Clinic)